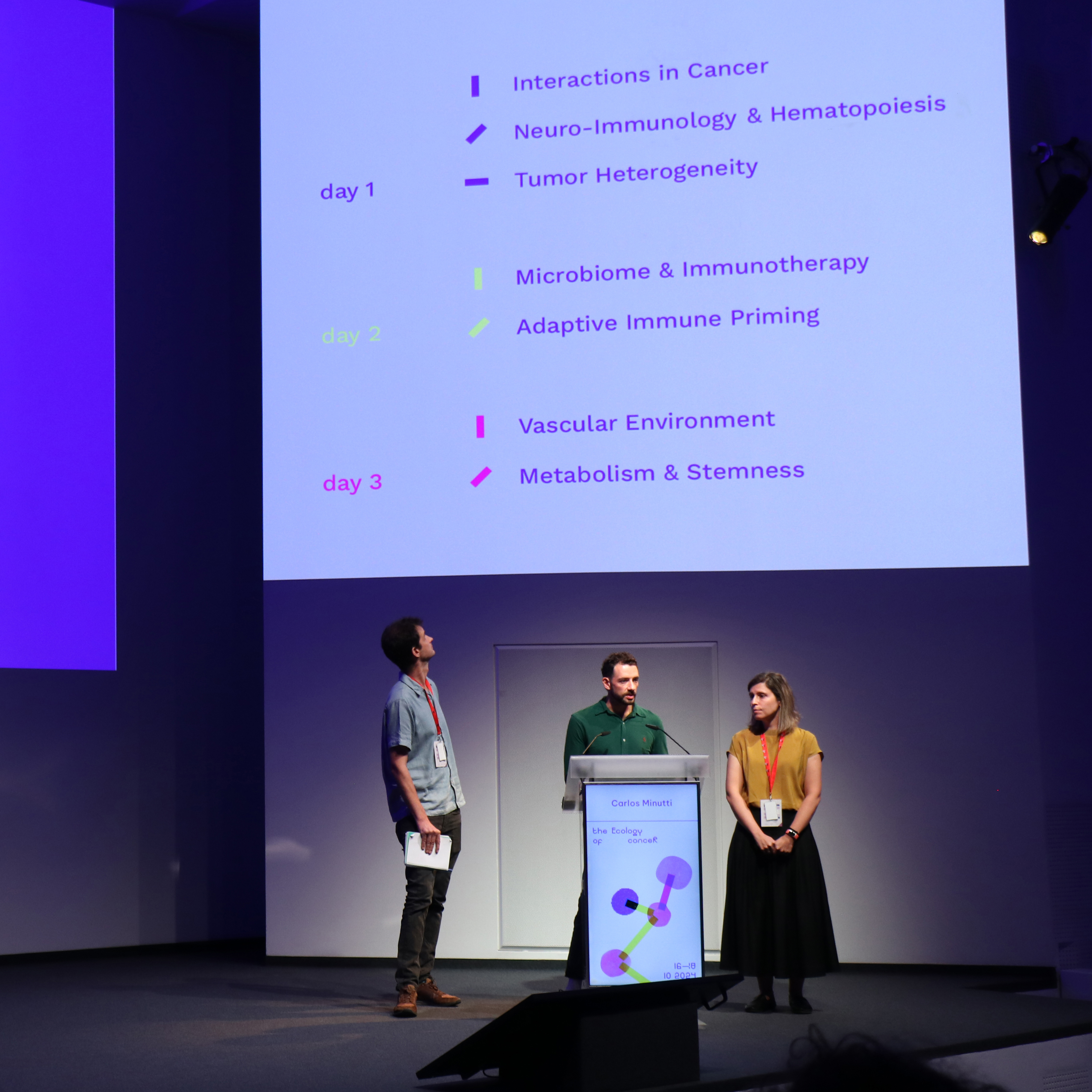
With nearly 30 presenters—including 4 keynote speakers—ranging from internationally renowned scientists to emerging researchers, the symposium was structured into eight thematic sessions, each exploring different dimensions, from the interplay between tumour cells and their microenvironment to the systemic impacts of cancer on the body.
Keynote Talks
Chaired by CF’s Principal Investigators Ana Luísa Correia, Carlos Minutti and Klaas van Gisbergen, the symposium opened with a keynote by Brian Brown from the Icahn School of Medicine, who discussed the challenges of immunotherapy resistance. He explained how spatial functional genomics, a method that shows which genes are active in specific areas of a tumour, can help identify why tumours escape immune attacks, leading to better immunotherapies.
Another keynote by Laurence Zitvogel of the Gustave Roussy Cancer Center shed light on how gut bacteria affect the body’s ability to fight cancer. Intestinal bacteria play a key role in how well certain cancer treatments, like immune checkpoint inhibitors, work, and antibiotics can reduce their effectiveness by disturbing this balance. Her research suggests that transferring faecal matter from patients who respond well to treatment could help others overcome resistance to immunotherapy.
Cyrus Ghajar from the Fred Hutchinson Cancer Center focused on dormant cancer cells that spread throughout the body but remain hidden from the immune system because they are so few in number. Understanding these cells is key to finding ways to prevent cancer from coming back.
Elaine Fuchs of The Rockefeller University explored how skin stem cells respond to environmental stresses like inflammation and cancer-related signals. These cells can “remember” past encounters, affecting how they respond to future challenges, which has implications for both healing and cancer development.
Themed Sessions
Among the eight sessions, a key focus was on how cancer impacts the formation of blood cells and immune responses. Discussions highlighted that tumours can send signals to the bone marrow, increasing the production of certain blood cells that help the tumour grow. This means tumours don’t just grow locally—they can reprogramme the immune system and blood cell production throughout the body to support their own survival.
Another key takeaway was that the nervous and immune systems are deeply connected, and their interactions can significantly influence how cancer develops and progresses. By using specially engineered mouse models, scientists are uncovering how cancer affects the nervous system, while other studies focused on how competition between cells in the thymus (a key immune organ) can impact the development of leukaemia.
Researchers also looked at how individual cells contribute to the start and growth of cancer. They shared how advanced imaging techniques allow them to see how mutated cells behave in living tissues, showing that the menstrual cycle can influence both the start of tumours and how they respond to chemotherapy. There was also discussion about how melanoma cells interact with their surroundings to maintain their “stem-like” state, which makes them more resistant to treatment. Another topic was how a protein called survivin helps skin stem cells kickstart the formation of basal cell carcinoma, a common type of skin cancer.
The symposium also explored the role of dendritic cells, which are immune cells that help kickstart the body’s defence against threats, including cancer. Different types of dendritic cells in the lymph nodes work together to influence the types of cancer-fighting T cells that enter tumours. Signals from the nervous system can affect the function of these immune cells, potentially boosting the body’s ability to fight cancer. Another presentation discussed how the immune system’s surveillance of tumours can shape the genetic makeup of cancer cells, which could lead to new cancer vaccine strategies.
How does the immune system learn to tolerate harmless substances? One talk introduced Thetis cells, a new type of immune cell that helps the body become tolerant to food and gut bacteria, which could have important implications for treating autoimmune diseases and cancer. Another talk discussed how CD8+ T cells, which are immune cells that attack infected or cancerous cells, are activated during viral infections. This knowledge could lead to improvements in vaccines and cancer treatments that use the body’s own immune cells.
A recurring theme was how tumours interact with their surroundings and evade immune detection. One talk revealed that bevacizumab, a drug known for blocking the growth of new blood vessels, also changes immune cells called macrophages within tumours, showing a new way the drug works. Another presentation discussed how lymphatic vessels, which help transport immune cells, influence the immune system’s ability to detect and fight tumours. Additionally, researchers found that changes in the cells lining liver tumours can block immune cells (CD8+ T cells), which may impact how well immunotherapy works.
The final session explored how ageing affects cancer development and treatment. Changes in the body's metabolism as we age can fuel cancer growth and spread, while also weakening the immune system’s ability to fight it. These findings highlight the importance of developing cancer therapies specifically tailored to older patients.
Looking ahead, #CRSy24 underscored the critical role of interdisciplinary collaboration in cancer research, gathering together researchers, clinicians, technologists, and patient advocates. Emerging tools like spatial functional genomics, single-cell RNA sequencing, and advanced imaging techniques are poised to help them dissect the complex interactions between tumours and the body with greater precision than ever before. By spotlighting these intricate interactions, #CRSy24 brought us a step closer to effective, personalised treatments that improve patient outcomes.
*The Champalimaud Foundation extends its gratitude to all the speakers, participants, sponsors and organisers who made #CRSy24 possible.
Text by Hedi Young, Science Writer and Content Developer of the Champalimaud Foundation Communication, Events & Outreach team.