Precursor lesions of pancreatic cancer are very difficult to characterise with magnetic resonance imaging (MRI). But now, in a new study, researchers led by Noam Shemesh and Carlos Bilreiro – respectively head of the Preclinical MRI lab at Champalimaud Research and a doctor at the Champalimaud Clinical Centre’s Radiology Department – have shown, for the first time, that a particular form of MRI, called Diffusion Tensor Imaging (DTI), is capable of robustly detecting pre-malignant lesions in the pancreas. Their study, which could open the way to early clinical diagnosis in people at risk, as well as to treatment assessment of pancreatic cancer, is published today (December 13, 2024) in the journal Investigative Radiology.
Pancreatic cancer is the third leading cause of cancer-related deaths in the US and the sixth in Portugal. When the disease is still localised, the estimated five-year survival rate is 44%, according to recent statistics from the US National Cancer Institute. But once it has metastasised, this figure goes down to around 3%.
Unfortunately, the symptoms of pancreatic cancer (stomach pain, unexplained weight loss, new-onset diabetes, jaundice, etc.) are non-specific and easily confused with those of other diseases. And when the symptoms appear, the cancer is, usually, already in an advanced, inoperable stage.
Ninety-five percent of pancreatic cancers are so-called pancreatic ductal adenocarcinomas (PDAC), and many of them develop from a precursor lesion called pancreatic intraepithelial neoplasia (PanIN). This makes detecting pre-malignant lesions for PDAC – that is, mainly PanINs – critical for diagnosing the disease at an early stage and for understanding PanIN biology.
Except that, contrary to what happens, for instance, with colorectal cancer, where cancer-precursor polyps are easily seen on a colonoscopy and removed, the problem with pancreatic cancer lies in the absence of non-invasive diagnostic tools for the early detection of PanINs. This also prevents the investigation of PanIN biology and of the genesis of pancreatic tumours in humans.
“Identifying precursor lesions for PDAC, mainly (...) PanINs, the authors write in their paper, “could provide opportunities for early diagnosis and development of more effective therapies.”
A new use for an existing method
However, they add, “PanINs are not diagnosed by current imaging modalities. (...) there is an urgent need for developing imaging methods for PanIN diagnosis and characterization, which could enable early diagnosis before PDAC is established”.
That was precisely the aim of the new study. And what the researchers found was that it is possible to detect PanINs using a form of MRI called diffusion tensor imaging, or DTI. “DTI is a method that relies on the diffusion of water molecules inside the tissues. Because the water molecules diffuse within the cells and experience interactions with cell walls and other microscopic objects, they serve as an endogenous tracer for tissue microstructure”, says Noam Shemesh.
Diffusion tensor MRI is typically used for imaging the brain, but that does not preclude its use in other organs. It was invented 30 years ago, so it is not new, which is a good thing if it is to be applied to human patients. “It's not a new method – it was just never applied in the context of pancreatic cancer precursor lesions”, notes Shemesh.
“It was Carlos [Bilreiro, first author of the study]”, he continues, “who came to see me with this idea”. They sat together and tried to figure out what MRI method could contrast PanINs, distinguishing them from simple, benign, pancreatic cysts. “We did a whole study on that with [co-author] Tânia Carvalho, from the Champalimaud Foundation’s Histology Platform. She was super helpful in this – we figured out that there are changes to the microstructure of the tissue due to these PaniINs. And in my lab, imaging microstructural changes is what we know how to do best”, Shemesh points out.
“This work was only possible due to the combined expertise of a multidisciplinary team of researchers led by Noam Shemesh, made up of radiologists and pathologists, MRI engineers and scientists, and veterinary pathologists”, adds Carlos Bilreiro.
Because the researchers embarked on this collaboration between scientists and clinicians with translation to the clinics in mind, the most efficient strategy was in fact to test a method that already exists, instead of developing something completely new – and unproven. “For translational purposes, it's always very useful and efficient if you can modify or adapt an existing method rather than develop one,” Shemesh explains. “Every MRI scanner already has this method implemented in it. It’s just the way we used it that is a bit new”.
The team was able to detect, using DTI, the microstructural changes that characterise PanINs in pancreatic tissue samples and in vivo for transgenic mice that are prone to developing these lesions. “Diffusion gives images a level of contrast that allows us to say, “oh, a PanIN is probably hidden in these pixels”, Shemesh points out.
Of mice and human samples
The researchers started by imaging transgenic mouse pancreatic tissue samples in one of the strongest MRI scanners in the world, which the Shemesh lab acquired in 2015: an ultrahigh-field 16.4 Tesla MRI machine. In comparison, 1.5T or 3T scanners are typically used in clinical practice.
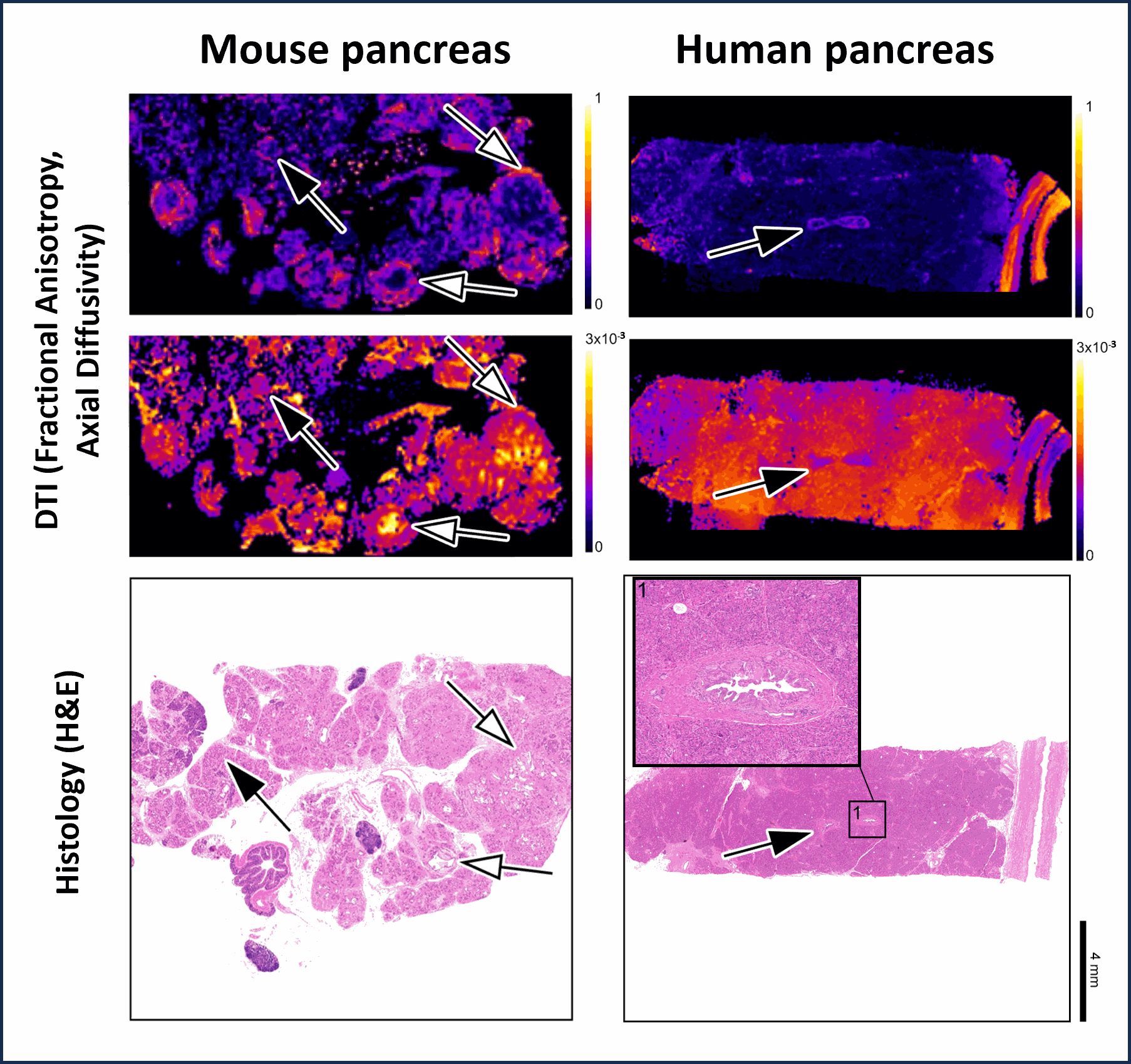
They then confronted the DTI images of each sample with the histological analysis of the same sample, to determine whether the lesions (microstructural changes) they saw matched the lesions seen in the histology of the samples. They matched – and very precisely so. Histology consists in the visualisation, under the microscope, of thin slices of prepared tissue (for instance, from a biopsy), to see the structure of cells and tissue and determine the nature of a tumour.
“Using the potentialities of the state-of-the-art MRI equipment we have in our laboratory, we managed to develop a magnetic resonance microscopy technique that enables us to directly compare the images obtained with histology slides”, says Carlos Bilreiro. “This technique allowed us to demonstrate that advanced diffusion imaging sequences – DTI – are capable of detecting pre-malignant pancreatic cancer lesions.”
The team further showed that the lesions could be detected in vivo in the transgenic mice. “We did this with our other big magnet, a 9.4 Tesla scanner”, Shemesh explains. “And actually, we also imaged the mice at multiple time points on a small 1 Tesla scanner we have”, which is equivalent to a clinical MRI machine.
Finally, they imaged human tissue samples. “We obtained samples from patients and showed that our results generalize to humans”, says Shemesh. “We took parts of human pancreases and scanned them in the same way we did the mouse samples. The histology and pathology of the samples showed that DTI was also efficient and effective for detecting human lesions.”
“Our work represents a proof of concept, and provides a basis to actually do a trial on humans, on patients with a method that is already basically implemented”, he concludes.
More studies are clearly needed for any future clinical use: “Technical differences between MRI in basic research and clinical imaging are obvious” the authors write, “and (...) loss of resolution [is] expected due to hardware constraints in clinical scanners and time constraints when imaging patients. Future studies should investigate if DTI can be used in clinical context for PanIN detection and characterization (...). Eventual combinations of DTI with other diagnostic tools could be used for increasing specificity, such as liquid biopsy and artificial intelligence.”
Concerning a future research/clinics collaboration, Shemesh is enthusiastic. “My research is in finding the contrast [in the images], but I'd be super happy to collaborate with medical doctors or radiologists that would want to look further into this and help them to map this on a bigger population. It's always very satisfying to know that something you've developed can help patients.”
He also emphasises the importance of such collaborations. “This project took years to develop. It took a lot of effort to develop the imaging in the transgenic mice, and Carlos and a technician from the lab, Francisca Fernandes, worked very hard on those. It was a huge effort and a huge amount of work. And I do think that it paid off in the end, and it ended up being really, really exciting.”
“I believe this study represents a milestone in research into premalignant pancreatic cancer lesions”, Carlos Bilreiro points out. “We are now able to detect these lesions in animals and better understand how pancreatic cancer develops. We also know that DTI is just as effective in the human pancreas. As for its clinical application, further studies will be needed to adapt the technique to the clinical context and to explore interventional or surveillance possibilities for pre-malignant lesions. This study thus represents a first step towards the early detection of pancreatic cancer with magnetic resonance imaging, even before the cancer develops.”
Original paper here.
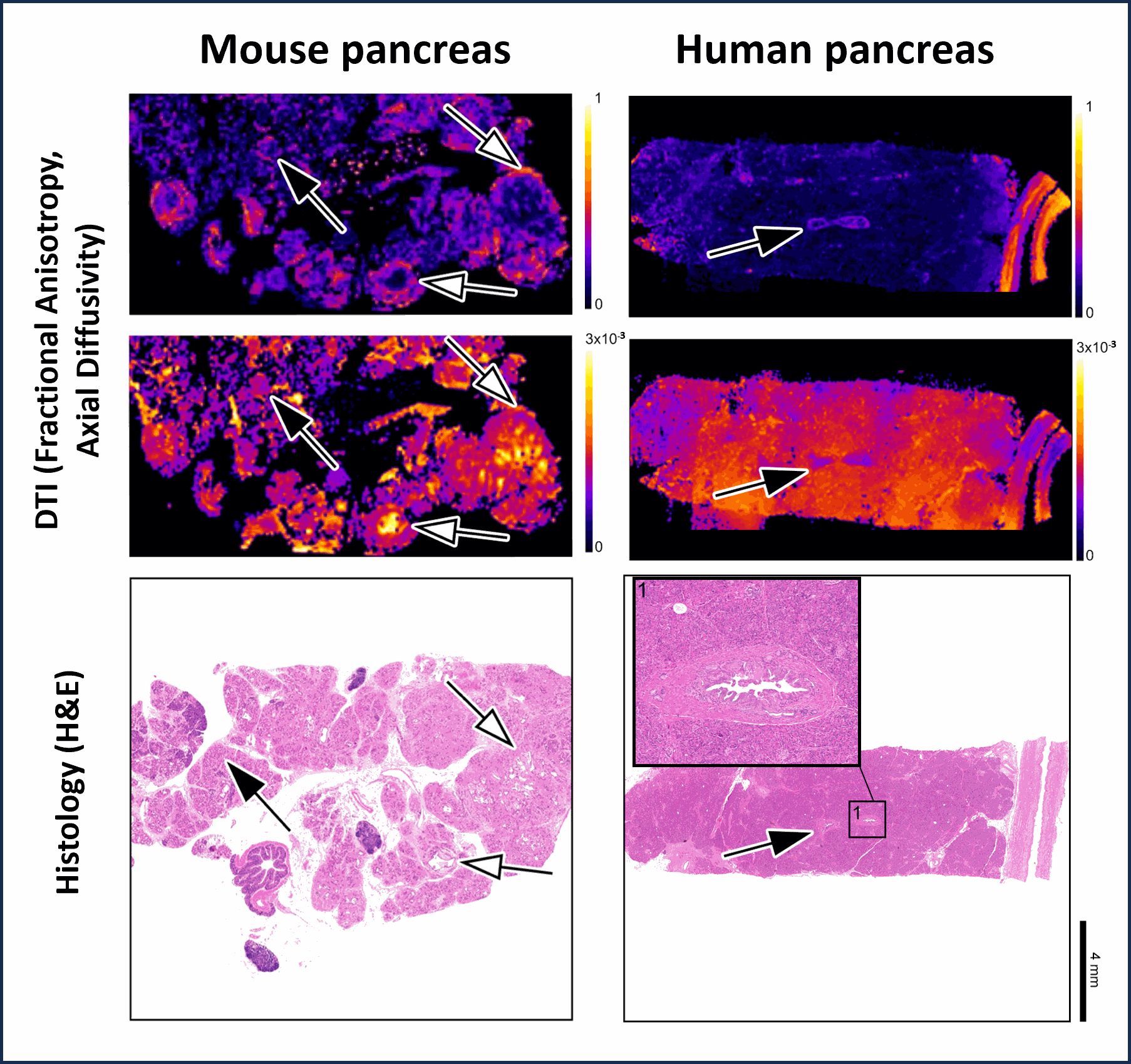
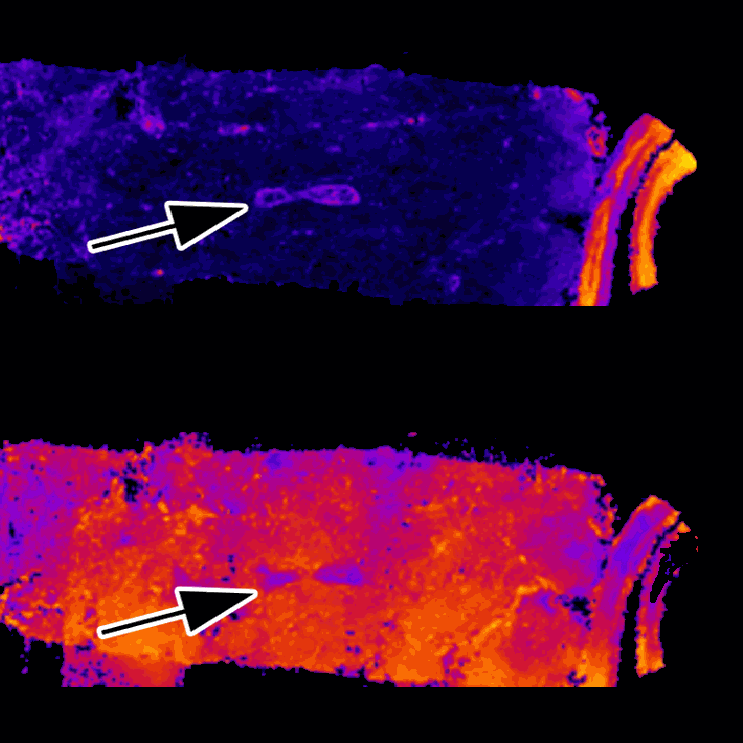
Image Caption
MRI microscopy of mouse and human pancreas with respective histology, demonstrating the ability of DTI maps (Fractional anisotropy and Axial diffusivity) to identify pre-malignant lesions (black arrows). The white arrows point to foci of adenocarcinoma.
Credit
Adapted from Bilreiro C, et al. Investigative Radiology, 2024.
Text by Ana Gerschenfeld, Health & Science Writer of the Champalimaud Foundation.